
“Is it possible that your vitamin D supplement may be secretly fighting your prescription medicines?” However, there are millions of Americans that have heart disease, high levels of cholesterol, and high blood pressure, taking this vitamin that is claimed to be absolutely necessary for the bones and immune system when they could be experiencing unwanted interactions with all prescription medicines.
Recent research studies, like that of 2025 TARGET D, suggest vitamin D as a vitamin which needs to be consumed in a tailored manner to lessen the chances of a heart attack by more than 50 percent. But it is vital to take into consideration the risks of vitamin D while consuming it to reap its benefits through incorrect medications.
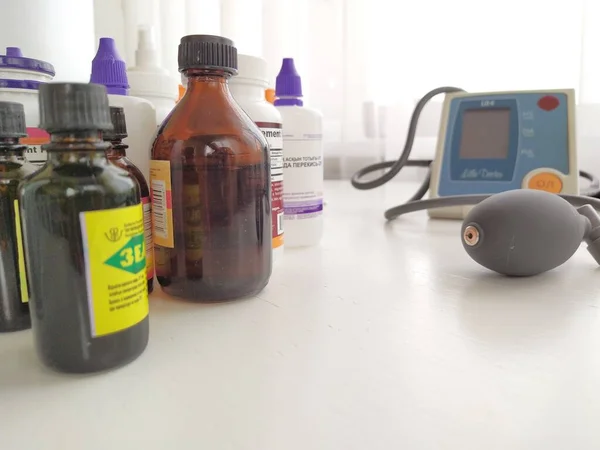
The following is a list of nine prescription and over-the-counter drugs with which vitamin D may interact, the relevance of the possible interactions, and some questions to ask your healthcare professional before taking the drugs in combination with the vitamin D supplement.

1. Statins
Statins include atorvastatin, lovastatin, and simvastatin, which act as inhibitors of HMG-CoA reductase, hence lowering blood cholesterol. For the body to synthesize vitamin D, cholesterol is necessary. An impact, therefore, might be expected from the lowering of blood cholesterol. But both the statin drug and vitamin D are metabolized in the body by an enzyme named CYP3A4, located in the liver. Thus, both might cause an increase in vitamin D. An inhibition, therefore, might be possible in statin drug levels.
In general, it gets a small response in terms of reduced cholesterol; though, it is recommended to monitor it, particularly when taken in large amounts of Vitamin D. There is a little evidence regarding the influence of Vitamin D levels in achieving an effective result of statins; however, no concrete clinical evidence has been presented.

2. Orlistat
Orlistat is sold under the trade name of either Xenical or Alli, as it inhibits the absorption of dietary fats in the intestines by preventing their re-absorption. Because it is a fat-soluble vitamin, the consumption of orlistat greatly inhibits the absorption of vitamin D in the body, which in turn leads to low levels in the blood. Prolonged use of the drug has been attributed to low levels of blood fat-soluble vitamins.
They will normally recommend the need to take vitamin D supplements, if possible at least two hours before or after the administration of orlistat, to avoid interference. It will facilitate sufficient vitamin D and will not hamper weight loss aims.
3. Thiazide Diuretics
Thiazides are a class of diuretics that include hydrochlorothiazide as one of their agents; they decrease the excretion of calcium in urine and increase blood levels of calcium. Vitamin D increases intestinal calcium absorption. The combination of these two medications can be associated with an increase in the risk of hypercalcemia, especially in older patients or those with impaired renal function.
And there was a post-hoc analysis involving an experiment on black patients, in which vitamin D3 at doses of up to 4,000 IU was given in combination with hydrochlorothiazide, and there was no significant increase in calcium, and even less frequent instances of hypercalcemia, but higher doses or longer treatment courses could possibly be cautiously used.

4. Corticosteroids
They are prednisone and dexamethasone; they suppress the absorption of calcium and are also recognized to stimulate the elimination of vitamin D activated by the pregnane X receptor. They cause the depletion of bones on minerals and make them brittle or weak. They are also sometimes the cause of osteoporosis.
The risk is higher when patients have low vitamin D. The condition can easily be alleviated through adequate monitoring and vitamin D intake, without there being any concrete evidence that shows the increasing impact of vitamin D on the anti-inflammatory properties of steroids in asthmatic patients.

5. Bile Acid Sequestrants
Cholestyramine, colesevelam, and colestipol work by binding to bile acids in the intestines, resulting in the elimination of these compounds from the body. This brings about a reduction in blood cholesterol levels. Bile acids facilitate the absorption of vitamin D. Hence, cholestyramine, colesevelam, or colestipol can cause an inhibition of vitamin D absorption.
The interaction could be minimized if vitamin D were taken at least four hours prior to the bile acid sequestrant dose, and this has been advised by experts since at least four hours would have passed before the drug’s mechanism of sequestration of bile acids and other nutrients.

6. Digoxin
Digoxin is employed in the treatment of atrial fibrillation and heart failure. The safety of the drug can be influenced by highly elevated levels of calcium in the body. Excessive levels of vitamin D, higher than the recommended daily limit of 4000 IU, can contribute to hypercalcemia. Severe hypercalcemia can result in dangerous arrhythmias.
Vitamin D in large quantities is a contraindication in patients on digoxin because it may lead to heart conditions because of excess calcium in the body.

7. Diltiazem
Diltiazem is another name that can be used for the treatment of HTN and some arrhythmia conditions. There is an association with metabolism because the analog of Vitamin D can increase the level of calcium, resulting in arrhythmia. Even though the likelihood of the event is low when regular doses of vitamin D are taken, a patient on concomitant treatment is to take extra care regarding the symptoms of the condition of hypercalcemia, which in turn could be muscle weakness and confusion.

8. Mineral Oil
Since it is an OTC product that has the role of coating in the intestines, the mineral oil hampers the body from absorbing water as well as hinders the body from absorbing fat-soluble vitamins. The two products would cause a decrease in the absorption of vitamin D. Since the use of mineral oil is short-term, these reactions are not very grave. Space between the administration, ensuring proper vitamin D is absorbed.

9. Supplements Containing Calcium & Magnesium
Both calcium and magnesium are commonly considered as SROs of vitamin D for strengthening bones, but when taken in higher amounts, there is an imbalance. When an excessive amount of calcium along with vitamin D is taken, there is an excessive level in the blood that causes grave consequences. An excessive level of vitamin D found in the body hampers the body from retaining calcium, leading to anemia.
When taken along with vitamin D, administration of calcium and magnesium supplements demands that these supplements be consumed after an interval that exceeds hours. Administration of leafy vegetables and nuts as magnesium supplementations is considered better since the body would take in higher amounts of that demanded mineral.
Vitamin D plays an extremely vital role in each and every manner as it deals with strengthening the bones. Fewer cases have been observed due to heart attacks and strokes, along with the consumption of Vitamin D. But interaction with various prescribed medicines goes into grave details. The nine cases listed below justify that interaction exists in each and every manner. Though certain interactions may have grave consequences, following the specialist’s instruction avoids adverse consequences despite interaction with vitamin D.


