Vitamin D is not necessarily safe in that it comes in the form of a supplement. When it is combined with a combination of medications containing prescriptions of cholesterol, blood pressure, heart rhythm, or chronic inflammation, the same nutrient as the one that helps to strengthen bone and muscle might alter the level of drugs, or alter absorption, or may elevate calcium levels, than desired.
That risk is likely to manifest in two ways: either vitamin D will not be able to be effective enough (thus, deficiency will not be eliminated), or it will be able to excessively increase calcium levels, which is important with some heart medications and in individuals who are already sufficient in calcium.
These drug combinations are so frequent that they warrant an intentional discussion with a practitioner, particularly when drug doses creep up or several acting drugs are all combined.
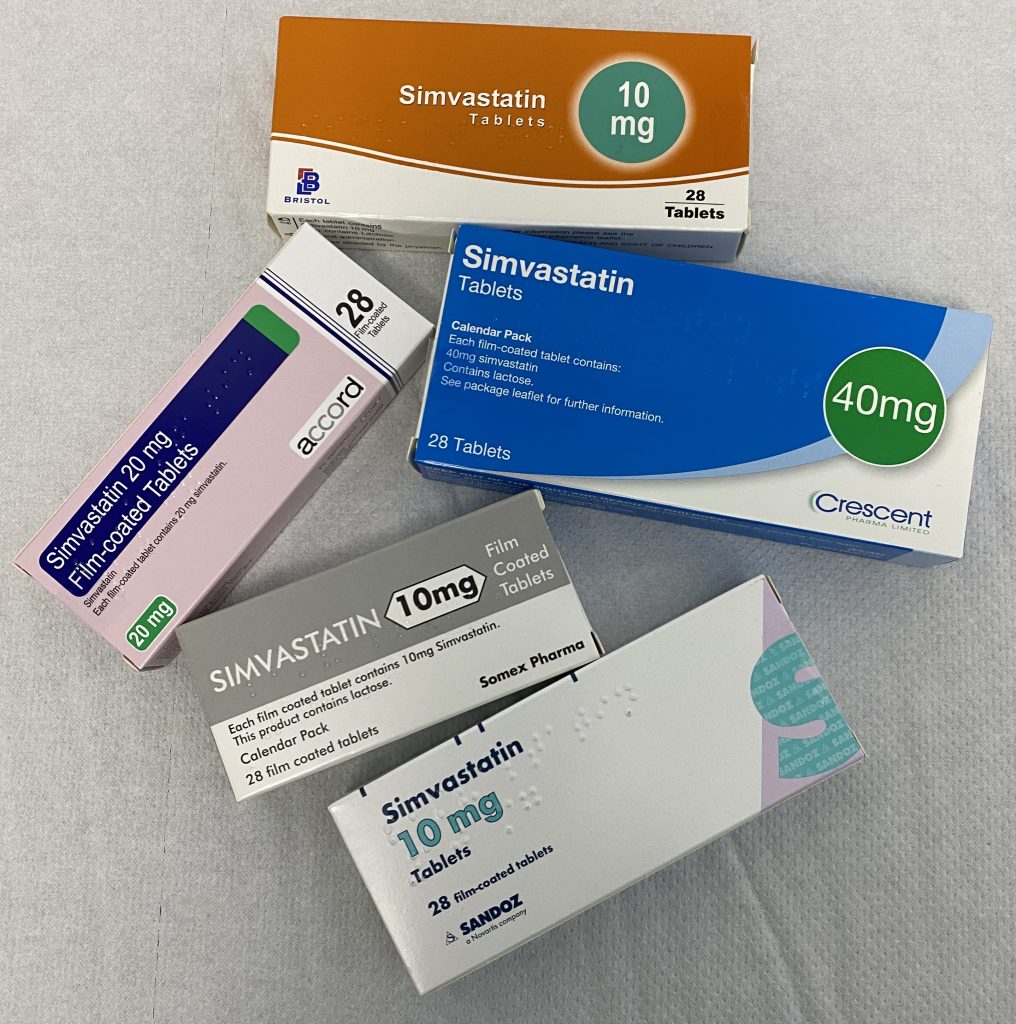
1. Statins (atorvastatin, lovastatin, simvastatin)
Other statins and vitamin D have a significant liver-metabolism route (CYP3A4) which causes competition that can alter the level of one or both. Practically, this may imply that the level of vitamin D increases, and the statin level decreases, which may make the effect of cholesterol-lowering agents dull in some individuals. The communication is not predictable person-to-person; that is the reason why it is more significant to be monitored with high doses of vitamin D in combination with long-term statin treatment.

2. Orlistat
Orlistat decreases the amount of fat that is absorbed in the gut and vitamin D requires the gut to absorb fats to enter the body. In the long run, this may reduce the status of vitamin D despite one taking a daily supplement. It helps with spacing doses, but even with persistent low levels they can still be found, especially when the diet already contains low levels of fat or the level of intake of vitamin D is marginal.
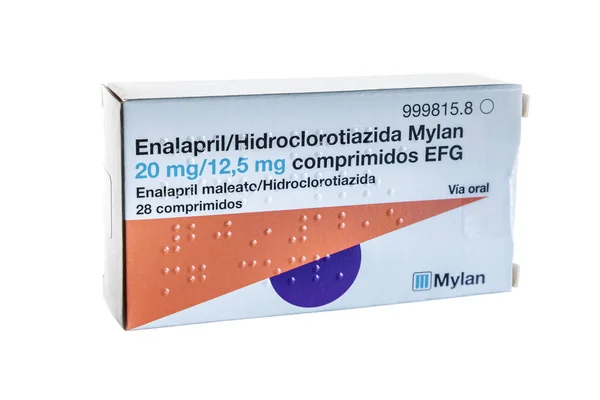
3. Thiazide diuretics (hydrochlorothiazide)
Thiazides decrease the urine calcium excretion, whereas vitamin D enhances intestinal calcium absorption. They are able to increase the chances of hypercalcemia together particularly in older adults and individuals with kidney conditions. The upper limit of intake has been cited in one instance as 4,000 IU/day since anything above that level would cause a shift out of range in calcium control.

4. Corticosteroids (prednisone, dexamethasone)
It is not a secret that long-term corticosteroids stimulate bone loss and part of that loss is due to decreased calcium absorption with a change in vitamin D processes. In that context, vitamin D receives a nomenclature of being protective, whereas the clinical nature of the issue is more complex: vitamin D can be beneficial, but dosing and monitoring have to correspond to the risks of fracture and baseline values. Meta-analysis of patients receiving corticosteroids showed a slightly significant bone loss prevention in spine and forearm with a weighted mean difference of 2.6 at the lumbar spine and 2.5 at the distal radius after one year with the combination of vitamin D and calcium.

5. Bile acid sequestrants (cholestyramine, colesevelam, colestipol)
These medicines reduce the level of cholesterol because they bind bile acids in the bowel, yet bile acids play a key role in the absorption of fat-soluble vitamins. Old studies demonstrated that cholestyramine decreases absorption of vitamin D which silently negativates supplementation. Timing separation is generally recommended, but what is of deeper concern is the fact that prolonged use of the vitamin may lead to a chronic deficiency of vitamin D unless the levels are monitored and the dosage is altered.

6. Digoxin
The safety margin of digoxin is low, and the elevated calcium concentrations may also predispose a person to rhythm disorders. Excessive intake of vitamin D to excessively elevate the calcium level may produce a situation similar to digoxin toxicity–clinically important since the initial manifestation may be uncharacteristic (fatigue, nausea) and then rhythm abnormalities develop. This is more alarming when vitamin D is taken along with the calcium supplements or with some drugs that already contain calcium.+
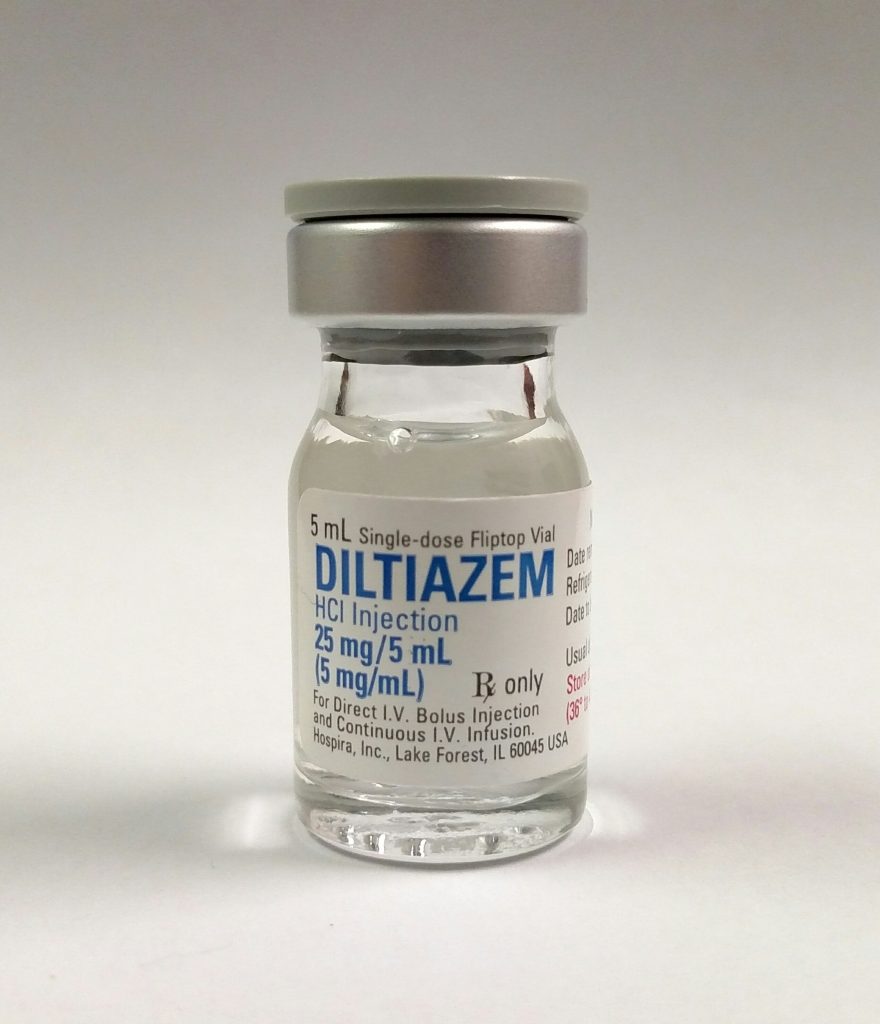
7. Diltiazem
Diltiazem is prescribed to treat hypertension and some arrhythmia, which is why electrolyte stability is especially significant. Vitamin D does not interact with diltiazem as some drugs have metabolism, but can indirectly cause arrhythmia when it helps raise calcium. The symptoms which indicate calcium has migrated to the high level like confusion, weakness, constipation or thirst should be addressed as a clinical red flag and not dismissed as an ordinary side effect.
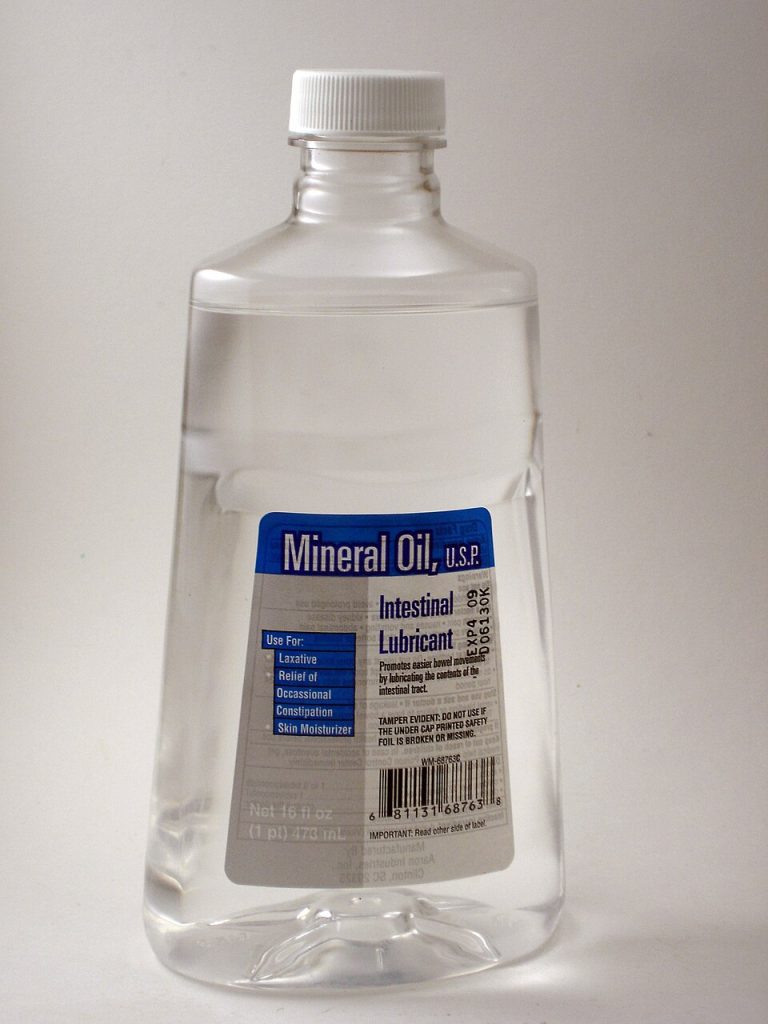
8. Mineral oil (laxative)
The intestinal lining may be covered by mineral oil and fat-soluble vitamin absorption may be impaired, such as that of vitamin D, although short-term use may not be a problem, but repeated use may cause an imbalance between what is on a label and what is actually being absorbed. To decrease interference, several hours should be allowed between the separation of mineral oil and vitamin D.

9. Calcium and magnesium supplements
Vitamin D enhance the absorption of calcium, but that is beneficial in the head of bone, but not good in situations where the total calcium intake is high or where thiazides, digoxin, or kidney failure are involved. Another contribution is made by magnesium as exceptionally large supplement doses may alter the calcium balance and complicate the interpretation of symptoms. The most reliable safety message of the long-term dosing data is that the more is better approach does not last long with vitamin D, particularly when dosages exceed 800-1000 IU/day taken in the form of the prevention of deficiency in the absence of lab advice.
Vitamin D may not be harmful, but it is more of a hormone than a vitamin supplement that can be safely added. In situations where the absorption, the metabolism of the liver is affected by medication, the safest method is to not list vitamin D as an independent medication but as a medication in the list. Regarding individuals undergoing any of the classes of the drugs listed above, the most important practical protective measure is straightforward: regular monitoring of vitamin D levels and calcium levels, along with dosing calculated to reach a preset target level and not a fixed high dose.


